Cost saving of switching to equivalent inhalers and its effect on health outcomes
Insights | 30/11/2020
Prescribing information available here
Adaptation from Bloom CI, Douglas I, Olney J, D’Ancona G, Smeeth L, Quint JK. Cost saving of switching to equivalent inhalers and its effect on health outcomes. Thorax 2019. 74 (11), 1078-1086
- Due to the high costs of asthma and chronic obstructive pulmonary disease (COPD) therapies, changing to a clinically equivalent less expensive option is often advocated. However, the impact of changing on patients’ health and healthcare utilisation has rarely been investigated in a real-world setting.
- This real-world study utilised UK primary care electronic healthcare records to assess the impact of inhaler change on health outcomes and treatment adherence of asthma and COPD patients, as well as to estimate potential cost-savings related to the change.
- Changing to a clinically equivalent inhaler in asthma and COPD did not negatively affect patient’s health or healthcare utilisation, such as the rate of general practitioner (GP) consultations.
- Switching to the least expensive equivalent inhaler in the cohort of regular inhaler users (n=665,105) would save around £6 million annually for the UK health economy.
In the UK, inhaler usage comprises a substantial healthcare cost. Due to high prevalence of asthma and COPD, three of the five most expensive medications in the National Health Service (NHS) budget are inhaler-delivered. Currently there are a wide range of therapeutic products available and switching to equivalent, but less expensive, inhalers is often advocated as a necessary cost-saving practice. Besides the cost, device environmental sustainability is another non-clinical reason to switch inhaler, among others. While randomised clinical trials have demonstrated comparable efficacy of treatment after a switch to an clinically equivalent inhaler, real-world studies assessing the health impact of inhaler switch in every day clinical practice are scarce.
This study utilised the UK primary care electronic healthcare records of asthma and COPD patients from years 2000–2016. Included in the analysis were those patients who were regular users of maintenance inhalers (ICS, LABA, LABA-ICS or LAMA) and who switched inhalers for financial reasons (no apparent clinical motivation) (n=69,812). Four different treatment outcomes were addressed: disease exacerbation, GP consultation, non-specific respiratory events, and adverse-medication events. The outcome rates were compared between the 3-month risk period following the switch and control periods (observed periods outside the risk period). The patients were divided into four cohorts depending on the outcomes experienced during the study (see figure 1). In addition, treatment adherence was compared using medication possession ratio (MPR) pre and post-switch, and the potential cost-savings related to the switch were estimated using 2017 NHS indicative prices.
According to the study, the prevalence of inhaler switch was low. From the identified cohort of 569,901 regular asthma inhaler users and 171,231 regular COPD inhaler users, only 2% and 6% had switched inhalers, respectively. Approximately two thirds of inhaler switches were made for non-clinical reasons. Inhaler switch was associated with reduced exacerbation rate; brand-to-generic, age-adjusted incidence rate ratio (IRR) 0.75 [95% confidence interval (CI) 0.64–0.88]; all other switches, age-adjusted IRR 0.79 [95% CI 0.71–0.88]. Differences in patient characteristics such as gender or condition (asthma/COPD), or inhaler-related factors such as therapeutic class or switch of device, metered dose inhaler (MDI) or dry powder inhaler (DPI), did not significantly affect the rate of exacerbations. Treatment adherence improved after the inhaler switch. This is possibly due to increased medication awareness related to the switch and may also explain the temporary reduction in the exacerbation rate. No significant switch-related change was observed in the rate of GP consultations, adverse-medication events or respiratory events. According to this study, switching of inhalers to the least expensive clinically equivalent inhaler in the total cohort of regular inhaler users in 2016 (n=665,105) would result in approximately £6 million savings annually for the UK health economy.1
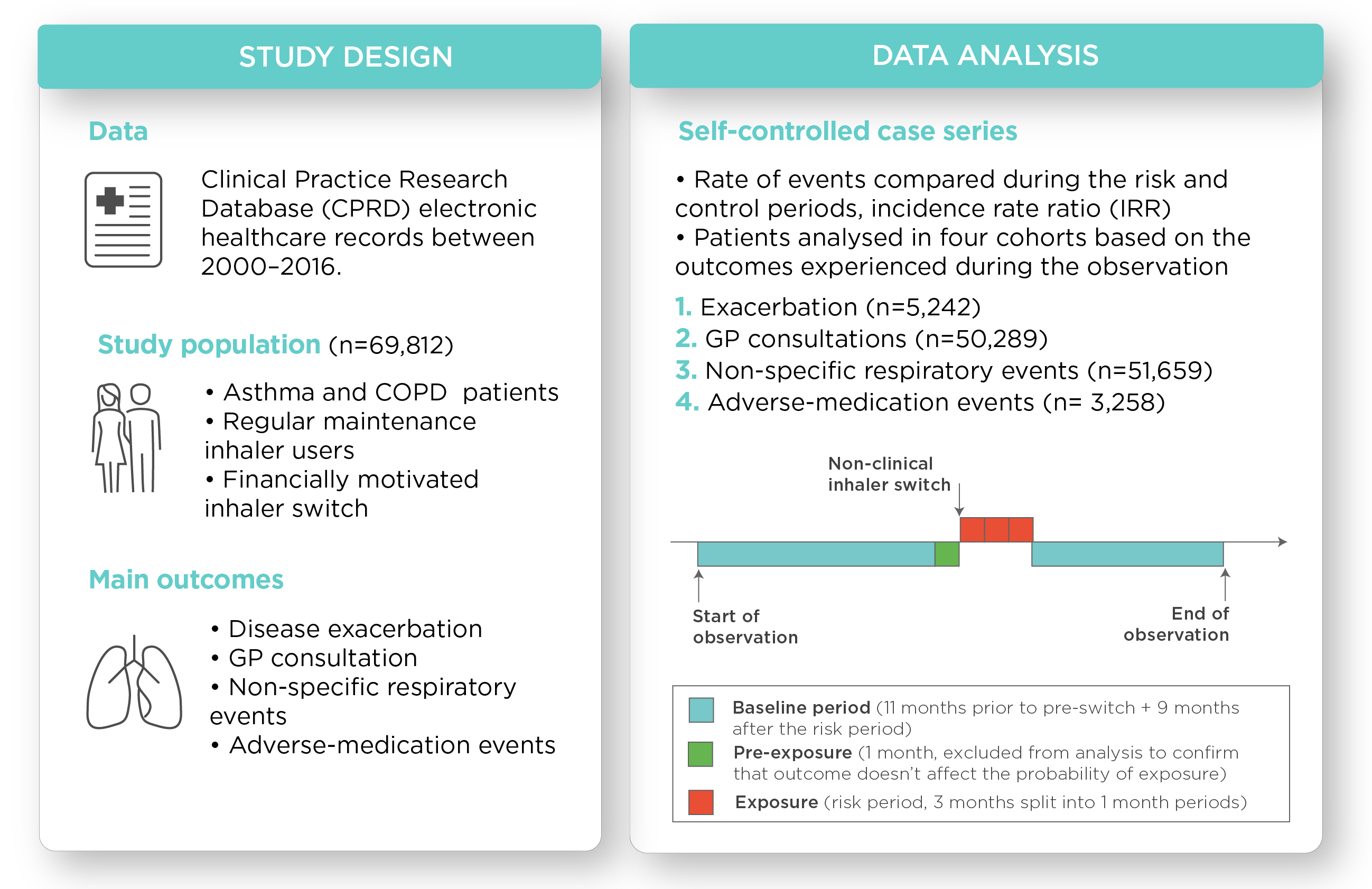
Figure 1. Summary of the study setting and data analysis
While inhalers are known to be a prominent healthcare cost, physicians may still be cautious in changing of patients’ inhalers in fear of losing disease control. This study suggests that a non-clinically motivated switch to an equivalent inhaler doesn’t impair patients’ health or increase healthcare professionals utilisation.1 In addition to cost savings, there are also other non-clinical motivations to change inhalers, one of which is concern for the environment. Moving from propellant-powered pressurised MDIs to more environmental-friendly options such as DPIs could significantly decrease the carbon footprint associated with asthma and COPD care.2 This study demonstrates good health outcome of non-clinically motivated inhaler switches in a real-world setting and supports the cost-saving clinical practice of changing to less expensive equivalent inhalers.1
Information to help in the discussion about inhaler device options is provided for asthma patients and health care professionals at the NICE website:
Read more about combating the climate change with a sustainable inhaler
Read more about Easyhaler® carbon life cycle assessment
Was this article helpful?
References
- Bloom CI, Douglas I, Olney J, D’Ancona G, Smeeth L, Quint JK. Cost saving of switching to equivalent inhalers and its effect on health outcomes. Thorax 2019. 74 (11), 1078-1086
- Wilkinson JK, Braggins R, Steinbach I, Smith J. Costs of switching to low global warming potential inhalers. An economic and carbon footprint analysis of NHS prescription data in England. BMJ Open 2019. 9(10):e028763
Adverse events should be reported. Reporting forms and information can be found at www.mhra.gov.uk/yellowcard. Adverse events should also be reported to Orion Pharma (UK) Ltd on
01635 520300.
August 2023 / RESP-690(1)

