Expert opinion paper: Improving asthma control with effective maintenance therapy can reduce both the risk of exacerbations and greenhouse gas emissions
Publikationer | 2025-07-29
A new expert opinion paper states that more sustainable asthma care, both for the patient and the environment, could be obtained by improving asthma control and choosing the right medications and inhaler types for individual patients1.
- Asthma care generates considerable emissions due to high healthcare resource use caused by poor asthma control2 and greenhouse gases used in pressurised metered-dose inhalers (pMDIs)3.
- Clinical experts stated that solutions to improve the sustainability of asthma care are already available; however, implementing change requires increasing awareness among healthcare professionals on the environmental impact of asthma management1.
- Asthma care should be shifted from rescue medication to preventive treatments that have a lower carbon footprint, to reduce both exacerbations and emissions1.
In this expert opinion paper, clinical experts representing seven European countries (Denmark, Finland, Germany, Italy, Spain, Sweden, and the United Kingdom) discussed potential solutions to challenges in achieving more sustainable asthma management. Two key factors were highlighted: enhancing asthma control by selecting the correct medication and choosing an appropriate inhaler device.
Treatment of asthma affects global greenhouse gas emissions in two major ways. First, propellants in widely prescribed pressurised metered-dose inhalers (pMDIs) are potent greenhouse gases that increase the carbon footprint of asthma care4. Second, poorly controlled asthma—characterised by acute exacerbations and hospitalizations—produces significant emissions due to increased asthma-related healthcare resource utilization1.
Poor asthma control across Europe was a shared concern, with clear overuse of short-acting b2-agonists (SABA) in many countries5. The authors argued that treatment of asthma should be shifted towards maintenance controller medications to reduce both the risk of exacerbations and the environmental impact of asthma care1.
The carbon footprint of pMDIs is known to be 20 to 40 times higher than propellant-free dry powder inhalers (DPIs) and soft mist inhalers (SMIs)6. Therefore, the choice of inhaler was noted as another key factor in reducing the carbon footprint of asthma care. Initiating treatment with DPIs or transitioning patients from pMDIs to DPIs could both lower emissions and improve asthma control1.
Local guidelines are important steering documents for healthcare professionals, however, many guidelines across Europe lack discussion on the environmental impact of inhalers. The authors emphasise that guidelines should be updated to recommend long-term preventive DPIs as the initial asthma treatment.1 The authors also raised concerns that resource shortages in European healthcare systems may compromise asthma care. Heavy healthcare resource utilization due to poorly controlled asthma, and related emissions, could be reduced by allocating more resources to early-stage asthma care, ensuring treatment balance.1
Key takeaways of the expert opinion paper are summarised in Figure 1. The experts conclude that solutions for sustainable asthma management already exist. However, successful implementation requires educating healthcare professionals and patients on the environmental impacts of asthma care, updating local guidelines, and investing in early asthma management.1
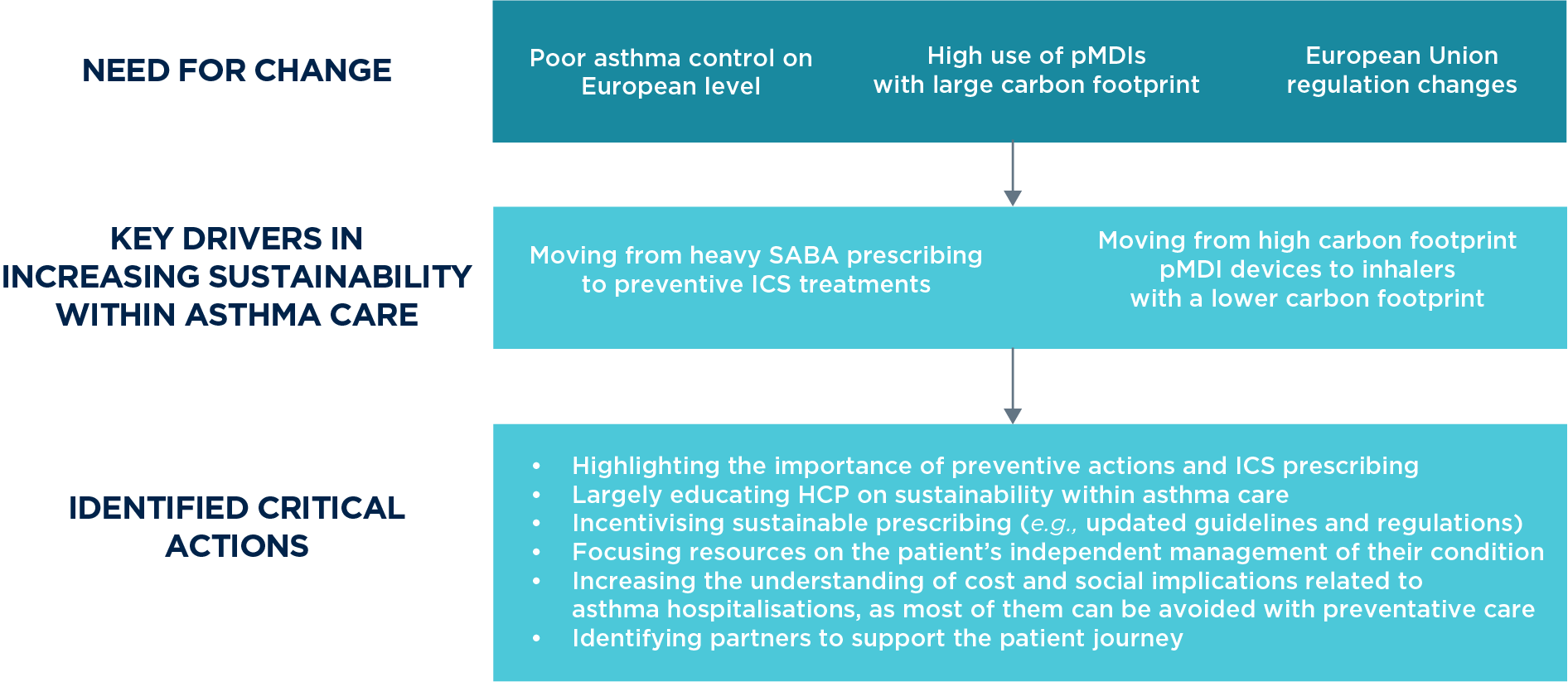
Figure 1. Key takeaways on how to improve asthma control and increase the sustainability of asthma care. The suggestions are based on the insights of the authors who represent seven European countries. HCP, healthcare professional; ICS, inhaled corticosteroid; pMDI, pressurised metered-dose inhaler; SABA, short-acting b2-agonists.
References:
- Janson C, Wilkinson A, Hisinger-Mölkänen H, Alcázar Navarrete B, Beeh K, Lavorini F, Kankaanranta H, Pritchard J, Suppli UC, Bansal A, Lähelmä S, Lehtimäki L. How to move towards more sustainable asthma care in Europe – Expert opinion paper. Breathe. 2025.
- Beeh K, Aumônier S, Whiting A, Fulford B, Mezzi K. Carbon footprint of severe asthma exacerbation management relative to Breezhaler dry powder inhaler. ERS Annual Congress 2021; Abstract 102.
- Fulford B, Mezzi K, Aumônier S, Finkbeiner M. Carbon Footprints and Life Cycle Assessments of Inhalers: A Review of Published Evidence. Sustainability. 2022; 14(12):7106.
- Tennison I, Roschnik S, Ashby B, Boyd R, Hamilton I, Oreszczyn T, Owen A, Romanello M, Ruyssevelt P, Sherman JD, Smith AZP, Steele K, Watts N, Eckelman MJ. Health care's response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021 Feb;5(2):e84-e92.
- Janson C, Maslova E, Wilkinson A, Penz E, Papi A, Budgen N, Vogelmeier CF, Kupczyk M, Bell J, Menzies-Gow A. The carbon footprint of respiratory treatments in Europe and Canada: An observational study from the CARBON programme. Eur Respir J 2022;60:2102760.
- Vartiainen V, Woodcock AA, Wilkinson A, Janson C, Björnsdóttir U, Haahtela T, Lehtimäki L. Thoughtful prescription of inhaled medication has the potential to reduce inhaler-related greenhouse gas emissions by 85%. BMJ Open Respir Res. 2024;11(1):e001782.

